This topic takes on average 55 minutes to read.
There are a number of interactive features in this resource:
 Human biology
Human biology
 Biology
Biology
 PSHE / Citizenship studies
PSHE / Citizenship studies
There are more than 400 million people worldwide who have diabetes and nearly 5 million of these live in the UK. Up to one in five people with diabetes are unaware that they have the condition.
Diabetes can be successfully managed, but the way this is approached depends on the type of diabetes. It has several long-term health effects. This is especially true if blood glucose levels are poorly controlled in an individual.
Type 1 diabetes is an autoimmune disease and accounts for up to 10% of diabetes cases in the UK. It typically develops before the age of 40 and occurs when the pancreas can no longer produce insulin.
There are two types of cells in the pancreas. Exocrine cells are responsible for the production and secretion of digestive enzymes. These pass along the pancreatic duct into the duodenum. These cells are not usually affected in diabetes. The pancreas also contains groups of cells called the islets of Langerhans. These cells release their products directly into the blood and so are a form of endocrine gland. Two hormones are produced in these islets. Insulin is made in beta cells and glucagon in alpha cells.
Type 1 diabetes develops when the person's own immune system destroys the beta cells. As a result insulin is no longer produced and blood sugar levels rise. This leads to the rapid onset of the symptoms of diabetes, including fatigue, unquenchable thirst, weight loss and the production of large volumes of urine. The risk of developing type 1 diabetes has recently been linked with genetic factors and may be associated with lifestyle factors such as diet and exercise.
Type 1 diabetes treatment can be complex and must be tailored to the individual patient. Injections of insulin are vital to keep sufferers alive. People with type 1 diabetes may require a number of injections of insulin every day, as well as (bolus) insulin. Type 1 diabetes patients should also receive advice on diet and exercise to support managing the disease.
Type 2 diabetes is a disorder that is increasing in both developed and developing nations as unhealthy diets and lifestyles become more common. It develops when the body can still make some insulin but not enough, or when the insulin that is produced does not work properly (known as insulin resistance). In most cases, this is linked with the person being overweight.
Type 2 diabetes usually occurs in people over the age of 40. In South Asian and African-Caribbean people, it often appears after the age of 25. Recently more children are being diagnosed with the condition. Type 2 diabetes is more common than type 1 diabetes accounting for 85-95% of people with diabetes.
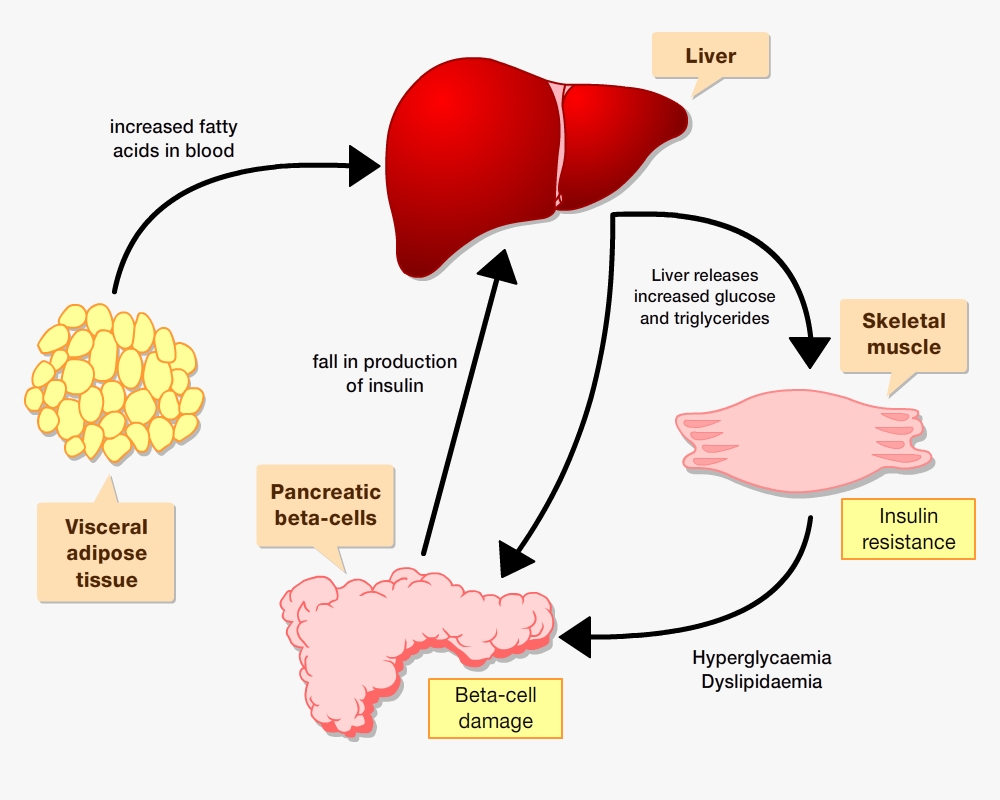
Many factors influence the development of type 2 diabetes; such as an inherited predisposition to diabetes and diets high in saturated fats, sugar and low in fibre. Being overweight also increases the chance of developing type 2 diabetes. Abdominal fat cells release fatty acids into the blood that stimulate the liver to release glucose and triglycerides. This process is therefore increased in overweight people with greater numbers of abdominal fat cells. Over a long period, muscles become insensitive to insulin and beta cells are destroyed.
Type 2 diabetes accounts for around 90% of cases in the UK. It typically develops in the over 40's and can be treated using combinations of lifestyle changes (diet and exercise), oral medicines and daily, long-acting insulin injections.
Healthy diet
Medicines
Regular exercise
Recent research has shown that it is possible to prevent diabetes in some people who are at high risk of developing the disease. For example, individuals in the Finnish Diabetes Prevention Study took part in an intensive lifestyle programme focussed on changing diet and physical activity behaviour. Over four years, these individuals were 60% less likely to develop diabetes than individuals who did not take part in the programme.
More detailed information on diabetes for young people