This topic takes on average 55 minutes to read.
There are a number of interactive features in this resource:
 Biology
Biology
 Human biology
Human biology
 PSHE / Citizenship studies
PSHE / Citizenship studies
 Science (applied)
Science (applied)
Communicable diseases cause millions of deaths globally every year. They are caused by pathogens and can be passed from one individual to another. A wide variety of organisms cause communicable diseases, ranging from tiny, geometric viruses to parasitic worms that can grow many metres long inside our bodies. The symptoms of disease result from how of our bodies respond to the invasion of these foreign organisms. Here is a summary of some of the features of common pathogens – to find out more see Pathogens and the immune system.
| Type of pathogen | Main features | Examples of disease |
|
Bacteria
|
Some bacteria invade and destroy the cells. Many produce toxins that cause disease. Endotoxins act locally, affecting the cells directly around the bacterium. Exotoxins are released into the body of the host as the bacteria grow and reproduce, travelling around the body causing disease. | Tonsillitis, septicaemia, pneumonia and tuberculosis (TB) |
|
Virus
|
Viruses are a combination of genetic material and protein that can invade living cells. They take over the biochemistry of the cells they invade to make more viruses, often destroying the host cells. | Common cold, influenza, chickenpox, polio, HIV/AIDS |
|
Fungi
|
Fungi do not cause many human diseases. There are a number of fungal skin conditions, and a few very serious conditions when a fungus attacks internal organs such as the brain or the lungs. | Athlete’s foot, ringworm, aspergillosis |
|
Protozoa
|
Protozoa act as parasites and cause human disease. They have two stages in their lifecycle so spend time in humans and another host that acts as a vector. | Malaria, amoebic dysentery, sleeping sickness |
To cure communicable diseases, medicines must either:
There are a number of different medicines that we can use against pathogens – but viruses and protozoa are very difficult to destroy.
Bacteria are prokaryotes and there are many features of prokaryotic cells that are different from our eukaryotic cells. Antibiotics are drugs that target bacteria and cure bacterial diseases. Many of their actions affect only bacterial cells, they either kill the bacteria or stop them growing but they do not destroy our human cells.
One way of classifying bacteria is by the way they take up Gram staining – they are known as Gram positive and Gram negative bacteria. The way they take up stain is affected by the structure of their cell walls. The structure of the cell walls also affects how sensitive a bacterium is to different antibiotics – there are some antibiotics that only affect Gram positive bacteria, and others that only affect the Gram negative species. The animation below demonstrates how the different antibiotics affect a bacterium.
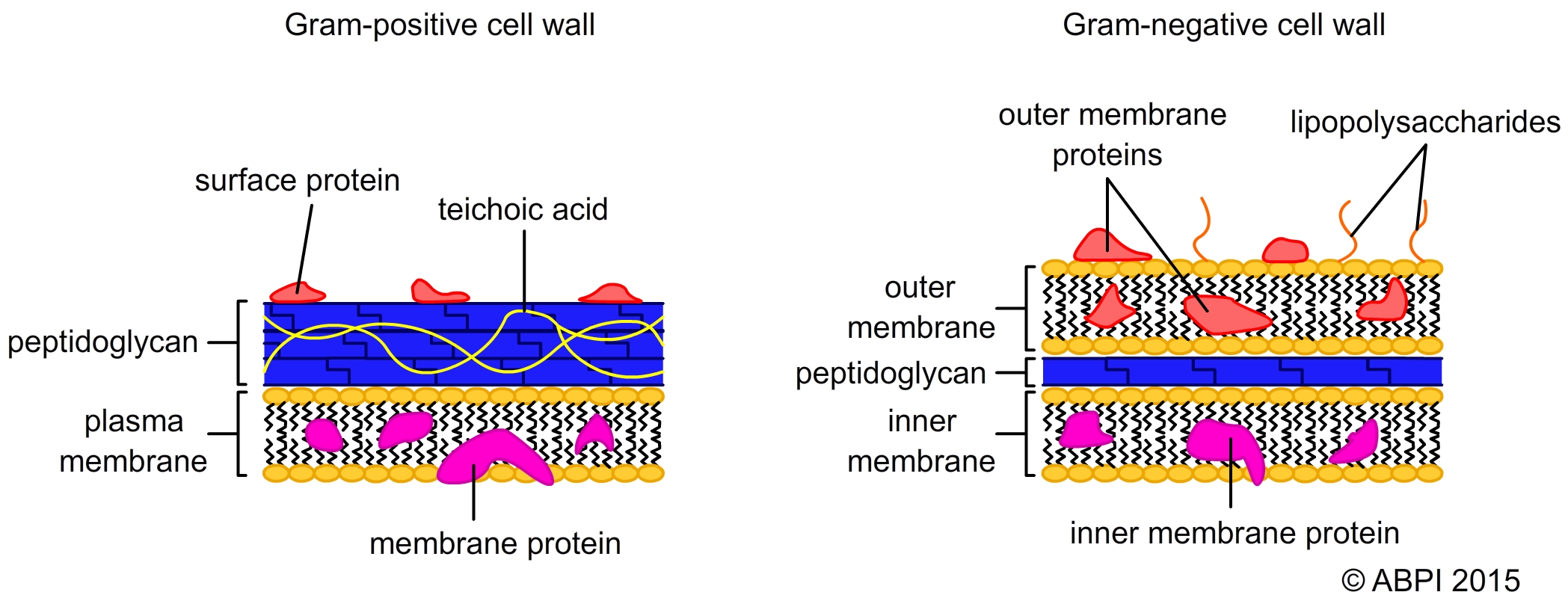
The structural differences between the cells walls of Gram positive and Gram negative bacteria affect the way they take up stain
– and the way they are affected by antibiotics
Some antibiotics are bacteriocidal – they kill the bacteria. Others are bacteriostatic – they prevent the bacteria from growing and this enables the immune system to recognise and destroy the pathogens. It will often depend mainly on the dosage used whether an antibiotic is bacteriostatic or bacteriocidal.
Some antibiotics affect a wide range of different bacteria. They are known as broad spectrum antibiotics. Others only destroy one or two species of bacteria – they are called narrow-spectrum antibiotics.
When antibiotics were first discovered and developed, people thought that infectious diseases caused by bacteria would become a thing of the past. There are a number of reasons why this hasn’t happened including:
Antibiotics are only effective if the target microorganism has a binding site for the drug or a metabolic process that the antibiotic interferes with. Mutations that arise during bacterial reproduction may result in phenotypic features that make the bacteria resistant to the drug. For example by making the cell wall impermeable to the drug, changing a biochemical pathway or the production of an antibiotic-destroying enzyme. These mutations will be selected for when the antibiotic is used as they enable the bacteria with the mutation to survive and reproduce when others around them are dying.
Antibiotic resistance has become a major problem – many common antibiotics are now almost useless in many developed countries. Some bacteria have developed resistance to many different antibiotics. If someone is infected by one of these multi-resistant bacteria, it can be a death sentence.
The animation below depicts how antibiotics work, how resistance to them arises and highlights the importance of completing a prescribed antibiotics course. Bacteria are not drawn to scale, i.e., in reality they are much smaller in relation to the size of the petri dish.
What is more, the numbers of new antibiotics being developed has been falling steadily. This is partly because it is becoming harder to find new compounds that are effective against bacteria, and partly because the potential financial return is lower because new antibiotics will be used very sparingly to try and avoid future resistance developing.
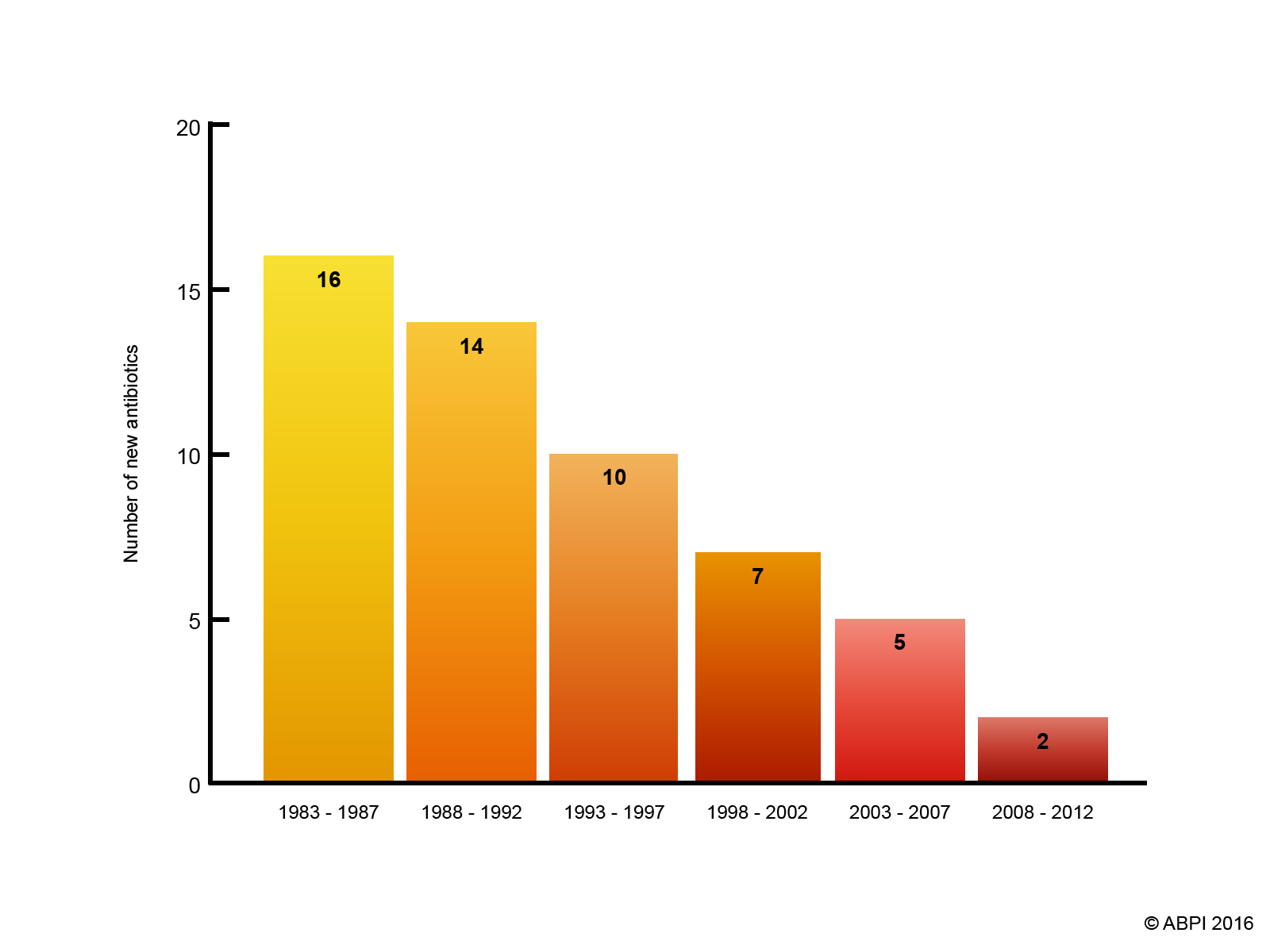
Graph showing the reduction in the numbers of antibiotics produced over time.
Controlling the use of antibiotics reduces opportunities for pathogens to develop resistance.
e-bug (www.e-bug.eu) is a free educational resource produced by Public Health England for classroom and home use and makes learning about micro-organisms, the spread, prevention and treatment of infection fun and accessible for all students.